
Preeclampsia is a serious and potentially life-threatening complication of pregnancy that affect 5-8% of US births. It typically develops after the 20th week of pregnancy, leading to high blood pressure and, in some cases, organ damage – most commonly to the liver and kidneys. That’s why recognizing preeclampsia first symptoms matters.
Preeclampsia can range from mild to severe, but its consequences can be serious for both you and your fetus if left undiagnosed or untreated. This is why recognizing early symptoms is crucial.
But how is preeclampsia diagnosed? Who can develop preeclampsia? What are the symptoms, causes, and risk factors?
In this post, we’ll address these and other questions, helping you identify early warning symptoms of preeclampsia. We’ll also explain how preeclampsia is diagnosed and treated, and when you should seek emergency care.
Whether you’re expecting, planning a pregnancy, or supporting someone who is pregnant, understanding preeclampsia could make all the difference to ensuring a healthy pregnancy and delivery.
Table of contents
What is Preeclampsia?
What Causes Preeclampsia
Who is Mostly at Risk of Developing Preeclampsia?
Identifying Preeclampsia Signs and Symptoms
When is Preeclampsia Diagnosed?
Preeclampsia Treatment
 What is Preeclampsia?
What is Preeclampsia?
Preeclampsia is a serious pregnancy-related condition characterized by high blood pressure, high levels of protein in the urine, and signs of damage to organs like the liver and kidneys.
It typically arises after the 20th week of pregnancy in women who previously had normal blood pressure. But it can also happen early or later in pregnancy, or even after delivery (postpartum or late postpartum preeclampsia).
While some cases are mild, this condition can progress rapidly and lead to serious complications, including:
- Preterm birth – when your baby is born before the 37th week of pregnancy.
- Placental abruption – when the placenta separates partially or completely.
- Stillbirth – when a baby dies in the womb at 20 weeks of pregnancy or later. It can happen before labor begins or during labor and delivery.
- Maternal and fetal death, if not properly managed.
Unfortunately, preeclampsia can develop suddenly and may not always present noticeable symptoms in its early stages. This is why regular check-ups are essential.
During prenatal care check-ups, your doctor monitors your blood pressure, urine protein levels, and general well-being. This helps them catch signs of preeclampsia, even if you don’t yet have symptoms.
 What Causes Preeclampsia?
What Causes Preeclampsia?
Although the exact cause of preeclampsia is not fully understood, research suggests it can originate from problems with the placenta’s development.
In a healthy pregnancy, blood vessels in the uterus expand to support the placenta and growing fetus. In women who develop preeclampsia, these vessels don’t develop properly, leading to reduced blood flow and high blood pressure.
Several factors may contribute to this abnormal development, including:
- Immune system dysfunction
- Insufficient blood flow to the uterus
- Genetic factors
- Existing conditions like chronic hypertension, obesity, diabetes, or kidney disease
Researchers also believe oxidative stress, inflammation, and poor placental implantation may play a role in triggering the cascade of events that lead to pregnancy preeclampsia.
Who is Mostly at Risk of Developing Preeclampsia?
Several factors can increase the risk of developing preeclampsia. While it can occur in any pregnancy, certain women are more likely to develop it due to underlying health or pregnancy-related conditions.
Higher risk for preeclampsia includes:
- First-time mothers
- A history of preeclampsia in pregnancy
- A mother or sister who had the condition
- Chronic high blood pressure (chronic hypertension)
- Gestational hypertension
- Preexisting kidney disease
- Diabetes (Type 1, Type 2, or gestational diabetes)
- Autoimmune conditions, such as lupus or antiphospholipid syndrome
- Multiple pregnancies (twins, triplets, or more)
- Obesity
- Older maternal age (risk increases for women over 35)
- Pregnancy through IVF or egg donation
- Long gap between pregnancies (more than 10 years between births)
Although these factors can increase your risk for preeclampsia or postpartum preeclampsia, no one is completely immune. This makes awareness of the symptoms of preeclampsia important for every pregnant woman.
Identifying Preeclampsia Signs and Symptoms
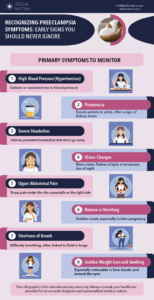
As mentioned, preeclampsia can begin silently, but recognizing its first warning signs and symptoms can make a critical difference in ensuring the safety of both you and your baby.
In its early stages, preeclampsia may not cause noticeable signs and symptoms. That’s why we always say that regular prenatal checkups are crucial.
At its first stage and even before you feel anything unusual, your healthcare provider might detect subtle changes, like elevated blood pressure or protein in your pee.
These early signs are red flags that your body may be starting to respond abnormally to pregnancy, particularly in how your blood vessels and organs are functioning.
So, here are the signs you should not ignore. Pay close attention to them, even if you feel generally well:
When is Preeclampsia Diagnosed?
Preeclampsia is diagnosed during your regular pregnancy checkups, and early detection is one of the most important parts of prenatal care.
Because symptoms can sometimes be subtle or mistaken for normal pregnancy discomforts or conditions like gestational hypertension, routine checkups are essential to diagnose preeclampsia.
Regular monitoring allows healthcare providers to spot early warning signs like high blood pressure disorders or changes in urine before the condition progresses.
Your doctor will assess your blood pressure, weight, urine, and overall symptoms at every prenatal visit. If preeclampsia is suspected, they will order further testing right away to confirm the diagnosis and evaluate how the condition is affecting your body.
What is the Screening Test for Preeclampsia?
Here’s an overview of the tests and procedures involved in diagnosis. These tests help determine the severity and guide your treatment:
Blood Pressure Monitoring:
High blood pressure hypertension is the most consistent and early measurable sign of preeclampsia. The key indicator of the disease is a blood pressure reading of 140/90 mm Hg or higher, taken at least twice, four hours apart.
Urinalysis (Protein Levels):
Your doctor will check a sample of your urine to measure protein levels. If protein is present (proteinuria), it may indicate that your kidneys are under stress. This test is often done using a dipstick during a routine visit or, for more accuracy, a 24-hour urine collection.
Blood Tests:
Blood samples assess how your organs are functioning and whether preeclampsia is impacting other organs.
>Kidney function tests
These check creatinine and uric acid levels.
>Liver function tests
Evaluation of liver enzymes (AST, ALT) for signs of liver stress or damage.
>Platelet count
A low platelet count could indicate a more severe form of preeclampsia, such as HELLP syndrome. HELLP stands for:
Hemolysis (breakdown of red blood cells)
Elevated Liver enzymes (a sign of liver stress or damage)
LP low platelet count (which affects the blood’s ability to clot)
HELLP syndrome symptoms may include nausea, vomiting, upper right abdominal pain, headache, and fatigue, sometimes overlapping with signs of preeclampsia.
If you’re diagnosed with HELLP syndrome, you’ll need urgent medical care and often early delivery to protect you and your baby.
Can You Have Preeclampsia Without High Blood Pressure?
High blood pressure is a hallmark of preeclampsia, so it’s typically required for diagnosis.
However, there are rare cases where the blood pressure may not appear elevated early on or may only be slightly elevated. Sometimes other serious preeclampsia symptoms develop first, such as protein in the urine, liver dysfunction, or low platelet count.
In the same way, not every woman who has gestational hypertension will necessarily develop preeclampsia.
Did you get a preeclampsia diagnosis? Don’t fret. Let’s explore the possible treatments next.
 Preeclampsia Treatment
Preeclampsia Treatment
Treating preeclampsia is about balancing the health and safety of both mother and baby. That said, the only true preeclampsia treatment is delivering the baby and placenta. However, treatment plans vary depending on how far along your pregnancy is and how severe the condition is. But first, a question we get asked quite often…
When Is Early Delivery Necessary?
In moderate to severe cases of preeclampsia, early delivery may be the safest option, even if it means the baby is born prematurely.
If the condition is putting your life or your baby’s health at serious risk, your doctor may recommend inducing labor or performing a C-section to prevent complications such as stroke, organ failure, or stillbirth.
How Early Will Doctors Deliver Due to Preeclampsia?
The timing of delivery depends on how advanced the pregnancy is and how well you and your baby are doing. In general:
- After 37 weeks of pregnancy: Delivery is typically recommended, even in mild preeclampsia cases, as the baby is considered full term.
- Between 34 and 37 weeks of pregnancy: Doctors may recommend early delivery if preeclampsia symptoms are worsening or severe.
- Before 34 weeks of pregnancy: Unless the condition becomes life-threatening, your healthcare team may try some strategies to manage symptoms and delay delivery to allow the baby more time to grow.
Treatment Considerations at Various Pregnancy Stages
As we mentioned, preeclampsia management looks different depending on how far along you are in your pregnancy:
At 32 Weeks Pregnant (Early Preterm)
The focus is on closely monitoring the pregnancy to prolong it safely while minimizing risks. You may be admitted to the hospital for frequent blood pressure checks, lab tests, and fetal monitoring.
If preterm birth is necessary, your doctor may recommend you take medications in addition to blood pressure drugs, such as corticosteroids to help your baby’s lungs mature more quickly.
You may also need to stay longer in bed and reduce your activities, though strict bed rest is less common today.
At 36 Weeks Pregnant (Late Preterm)
Because the baby is close to full term, doctors are more likely to recommend planned delivery to avoid progression or severe preeclampsia complications. If symptoms are stable, they may watch a little longer.
Ongoing Management
If you’re not yet ready for delivery, management may include:
- Antihypertensive medications to control blood pressure.
- Frequent lab tests to monitor kidney, liver, and platelet levels.
- Fetal monitoring to ensure your baby is growing well and not in distress.
- Regular ultrasounds and nonstress tests (NSTs).
Your care team may also advise lifestyle adjustments, close observation, and a detailed delivery plan if your condition worsens. These lifestyle adjustments are also useful to prevent preeclampsia or manage postpartum preeclampsia.
Managing preeclampsia requires a careful, individualized approach. With prompt medical care and regular monitoring, many pregnant women can prevent preeclampsia – or deliver healthy babies even if they have preeclampsia.
 When to Seek Emergency Care for Preeclampsia?
When to Seek Emergency Care for Preeclampsia?
Preeclampsia can progress quickly and become life-threatening if not treated. It’s essential to recognize when symptoms may signal an emergency. If you experience any of the following, seek immediate medical attention or go to the emergency room (ER):
- Severe or persistent headache that doesn’t go away with rest or medication.
- Changes in vision, such as blurred vision, flashing lights, or seeing spots.
- Severe pain in the upper right abdomen (under the ribs).
- Sudden and significant swelling, especially in the face, hands, or around the eyes.
- Shortness of breath or chest pain.
- Seizures (a sign of severe preeclampsia and eclampsia, a medical emergency).
- Decreased or no fetal movement.
- Heavy bleeding or signs of labor before 37 weeks.
- High blood pressure readings (especially 160/110 mm Hg or higher).
If you’re pregnant and something feels wrong, even if you’re unsure, don’t wait. Trust your instincts and contact your healthcare provider or visit the ER. With preeclampsia, early and decisive action are key here.
Recovery after preeclampsia often includes monitoring your health, managing lingering symptoms, and seeking emotional support to help you heal physically and mentally.
But recognizing the first symptoms of preeclampsia could save a life.
Prenatal care plays a vital role in detecting preeclampsia complications early, including preeclampsia and postpartum preeclampsia.
 Stella Mattina Can Manage Preeclampsia First Symptoms
Stella Mattina Can Manage Preeclampsia First Symptoms
If you’re pregnant and experiencing symptoms like swelling, severe headaches, or high blood pressure, don’t wait. At Stella Mattina, our Maternal Fetal Medicine specialists are experts in managing high-risk pregnancies and will monitor your pregnancy to keep you and your baby safe.
To schedule a prenatal visit or request a referral to our MFM specialists, call us today.
Dr. Krum is currently in practice in Arlington, TX. He received his undergraduate degree at Texas A&M University, then attended UTMB Galveston for medical school, finishing in 1986, completing his residency there in 1990. Providing a full range of obstetrical and gynecological care, he specializes in the treatment of endometriosis and robotic surgery. He arranges his schedule so that same-day appointments are usually available.
 What is Preeclampsia?
What is Preeclampsia? What Causes Preeclampsia?
What Causes Preeclampsia?
 Preeclampsia Treatment
Preeclampsia Treatment When to Seek Emergency Care for Preeclampsia?
When to Seek Emergency Care for Preeclampsia? Stella Mattina Can Manage Preeclampsia First Symptoms
Stella Mattina Can Manage Preeclampsia First Symptoms