Cervical cancer screening is important to safeguard your health, yet you may have questions about it.
What exactly is cervical cancer screening? Can a Pap test (or Pap smear) detect human papillomavirus (HPV)? How does an HPV test differ from a Pap test? What is HPV and how can it lead to cervical cancer if left undetected?
By highlighting the benefits of using both Pap tests and HPV tests, we aim to demystify the cervical cancer screening process. We’ll also guide you through interpreting your Pap smear and HPV test result – because regular cervical cancer screening is the most effective way of preventing cervical cancer.
Table of contents
Understanding Your Cervical Health and HPV
What is HPV?
What is Cervical Screening?
Who Should Get Cervical Screening?
Understanding Your Test Results
What Happens If You Have an Abnormal Test Result?
Understanding Your Cervical Health and HPV
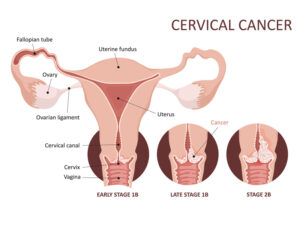
The cervix, located at the lower part of your uterus, plays a crucial role in your reproductive and overall health. It acts as a gateway between your uterus and your vagina, supporting pregnancy and allowing menstrual blood to flow out of your body.
So, keeping your cervix healthy is essential for maintaining fertility and reducing the risk of infections or cancers.
Cervical cancer is primarily caused by persistent infections with high-risk HPV strains, which can cause abnormal cell changes over time. These changes often go unnoticed because they rarely produce symptoms in their early stages.
That’s why regular cervical screening is so important, as it’s the most effective way to detect these changes before they progress or perhaps develop into cervical cancer.
Now, let’s learn about the most common cause of cervical cancer: HPV.
What is HPV?
Human Papillomavirus (HPV) is a group of more than 200 related viruses, some of which are sexually transmitted (it’s an STD). While most HPV infections are harmless and go away on their own, certain types of HPV are high-risk because they can cause cancers, including cervical, anal, and throat cancers.
How is HPV Related to Cervical Cancer?
Despite being common, some types of HPV are the leading cause of cervical cancer, responsible for nearly all cases.
When your body cannot clear a high-risk HPV infection, it can persist and cause cervical cell changes. Over time, these cervical cell changes may develop into precancerous cells (dysplasia) or cervical cancer.
This relationship between HPV and cervical cancer is particularly strong with two high-risk types of HPV, which cause about 70% of cervical cancer cases globally. These two strains are:
- HPV 16
- HPV 18
So, women with HPV 16 or 18 infections may require closer monitoring, even if their Pap test results are normal, due to the higher risk associated with these strains.
Other high-risk types of HPV include HPV 31, 33, 45, 52, and 58, which also pose significant risks.
For this reason, when an HPV test is positive, it’s important to identify its specific strain. Your doctor does that through genotyping – a test that provides critical information for assessing your risk of cervical cancer.
Understanding the type of HPV infection helps healthcare providers personalize screening and treatment plans, ensuring timely follow-up and better outcomes for your cervical health.
Now, let’s get to cervical cancer screening.
What is Cervical Screening?
Cervical cancer screening is a medical procedure that detects abnormalities in the cells of the cervix. It’s not a diagnostic test for cancer but rather a preventative measure to identify early changes in cervical cells that could develop into cancer if left untreated.
There are two primary types of cervical screening. We will explore each of them and the differences between them below:
- Pap Smear (or Pap Test): Identifies abnormal or precancerous cells in the cervix.
- HPV Test: Detects the presence of the human papillomavirus (HPV) that can lead to cervical cancer.
Pap or HPV Test, Which One to Choose?
While the HPV test and Pap test serve different purposes, they complement each other in safeguarding cervical health.
That means that instead of choosing one of them, using both ensures a more thorough screening approach. This enables earlier detection, better prevention, and increased peace of mind.
Here’s a brief overview of Pap and HPV tests:
HPV Test
The HPV test identifies the presence of high-risk strains of the human papillomavirus (HPV), particularly those most likely to cause cervical cancer, such as HPV 16 and 18. The purpose of this test is to detect high-risk HPV strains before any cell changes occur.
The procedure is simple. During a consultation and a pelvic exam, your doctor collects a sample of cells from your cervix with a small brush or swab. They send the sample to a laboratory where the pathologist analyzes and determines if there’s a high-risk strain of HPV present, or not.
A positive result indicates the presence of high-risk HPV, prompting closer monitoring or additional tests.
Pap Test
A Pap smear, also known as a Pap test, is a screening procedure that checks for abnormal cell changes in your cervix. Unlike the HPV test, a Pap test does not directly test for HPV, but it can reveal changes in cervical cells often caused by an HPV infection.
In many cases, an HPV test is performed alongside a Pap test (co-testing) for a more comprehensive assessment.
The Pap test is named after Dr. Georgios Papanikolaou, a Greek physician who pioneered this screening method in the 1940s. It revolutionized the early detection of cervical cancer and remains a cornerstone of women’s health care.
Its primary goal is to identify precancerous or cancerous cells early, enabling timely treatment and reducing the risk of cervical cancer.
The procedure is simple, quick, and similar to the HPV test. During a pelvic exam in your gynecologist’s office, your doctor will gently insert a speculum into your vagina to widen it. This provides access to your cervix, and they use a small, soft brush or spatula to collect cells from the surface of the cervix.
Your doctor sends the sample to a laboratory for analysis to detect abnormal or precancerous changes, known as dysplasia.
Who Should Get Cervical Screening?
In general, women between the ages of 21 and 65 should get regular cervical screening, as it’s the most effective way to prevent cervical cancer, but this may vary according to factors like individual health history.
Health authorities, including the American Cancer Society (ACS), have established guidelines to ensure timely and effective screening for individuals at risk.
If you’re unsure about your screening needs, consult your healthcare provider to create a personalized plan, but here are the latest recommendations based on guidelines from the ACS and other health organizations:
Ages 21-29:
Test: Pap test only.
Frequency: Every 3 years.
HPV Testing: Not routinely recommended, as HPV infections in this age group are often low-risk and resolve on their own.
Ages 30-65:
Preferred Option: Co-testing (Pap test + HPV test) every 5 years.
Alternative Options: HPV test alone every 5 years. Pap test alone every 3 years.
Ages 65 and Older:
Stop Screening: If there’s a history of adequate prior screening with normal results and no history of high-risk conditions.
Continue Screening: If risk factors are present, such as a history of cervical precancer or inadequate primary HPV testing.
After a Hysterectomy:
Without Cervix Removal: Follow the same guidelines based on age and risk factors.
With Cervix Removal: Screening is not needed unless there’s a history of cervical cancer or precancer.
Individuals Vaccinated Against HPV:
Even if vaccinated, follow the same guidelines, as the vaccine does not cover all high-risk HPV strains.
Higher-Risk Individuals:
Women with weakened immune systems (e.g., those with HIV or on long-term immunosuppressive therapy) may require more frequent screening.
Pregnant Women:
Cervical screening can be safely performed during pregnancy if needed, though the timing may be adjusted based on individual circumstances.
Understanding Your Test Results
Cervical screening results provide critical insights into your cervical health and cell changes. While normal results bring reassurance, abnormal results can be confusing and concerning.
Knowing what these results mean – and the steps to take – can help you stay calm and proactive about your health. So, here’s what you should expect:
Normal Test Results
Pap Test: Normal Pap test results indicate no abnormal cervical changes in cells. In that case, follow routine screening guidelines for your age and risk level.
HPV Test: A negative HPV test result means no high-risk HPV strains were detected. You can continue regular screening as recommended.
Abnormal Pap Test Results
An abnormal Pap test means some cervical cells appear unusual but do not necessarily indicate cancer.
But does an abnormal pap smear mean HPV? Can you have an abnormal pap smear without HPV?
Yes, you can. An abnormal Pap test often points to the presence of HPV, but it is not a definitive diagnosis of HPV.
If your Pap test results are abnormal, your healthcare provider will likely perform further testing, including HPV tests, to determine the cause of the abnormality and the appropriate next steps.
Regular screening and follow-up care are crucial to monitor and prevent the progression of HPV-related cell changes in your cervix.
To help you understand the connection between abnormal Pap tests and HPV, you can check the classification of abnormal results based on the severity of the cell changes…
Classification of Abnormal Results
ASC-US (Atypical Squamous Cells of Undetermined Significance):
This result indicates mild cervical cell changes, often caused by HPV or other benign conditions. You may need to take additional HPV testing to determine if high-risk strains are present.
LSIL (Low-Grade Squamous Intraepithelial Lesion):
LSIL indicates mild, often temporary cell changes typically linked to HPV. If you get abnormal HPV cells in a Pap smear, or if you get a positive primary HPV test, your doctor may require some follow-up testing to monitor the changes.
HSIL (High-Grade Squamous Intraepithelial Lesion):
This indicates more severe cell changes with a higher risk of progression to cancer. If you get this result, your doctor will require further evaluation, such as a colposcopy (see below) and biopsy.
ASC-H (Atypical Squamous Cells, Cannot Exclude HSIL):
This result suggests abnormal cervical cells that might be precancerous. In that case, a colposcopy is usually recommended for further investigation.
AGC (Atypical Glandular Cells):
That indicates abnormalities in the glandular cells, which may signal precancerous changes or cancer in the cervix or other areas. This result requires additional testing.
Abnormal HPV Test Results:
A positive HPV test indicates the presence of high-risk HPV strains, but this does not necessarily mean cancer is present.
The next steps depend on additional factors, like your primary HPV testing, age, and medical history. But if HPV 16 or 18 is detected, you’ll need immediate follow-up with another Pap test and a colposcopy.
What Happens If You Have an Abnormal Test Result?
Receiving a positive result for abnormal cervical cells can be concerning, but it’s essential to understand what it means and the steps for follow-up care.
Most abnormal cervical cells do not indicate cancer but highlight the need for closer monitoring or treatment to prevent progression.
Here are some possible follow-up alternatives after an abnormal result:
Colposcopy: If you get a positive result, your doctor may require a colposcopy, a procedure to closely examine the cervix, vagina, and vulva using a colposcope (a magnifying instrument).
Biopsy: If your doctors find abnormal areas during the colposcopy, they will take a small sample of cervical tissue for laboratory analysis. Types of biopsies include:
- Cervical biopsy: Removes a small section of the abnormal area.
- Endocervical curettage (ECC): Scrapes abnormal cells from the cervical canal.
Possible Outcomes of Abnormal Test Results
Precancerous Changes (CIN):
- CIN 1 (low-grade changes): Often monitored with repeat Pap and HPV tests, as they may resolve naturally.
- CIN 2 or 3 (moderate-to-high-grade changes): Requires treatment to remove or destroy the abnormal cells.
Treatments for precancerous changes include:
- Cryotherapy: Freezes the abnormal cells to destroy them.
- LEEP (Loop Electrosurgical Excision Procedure): Uses a wire loop heated by an electric current to remove abnormal tissue.
- Cone biopsy: Removes a cone-shaped piece of cervical tissue for further examination and treatment.
- Laser therapy: Uses a laser to remove or destroy abnormal cells.
Cervical Cancer Diagnosis:
Cervical cancer-positive results are rare in women who follow a regular cervical screening schedule of HPV test and Pap smear – but are possible in advanced cases. Cervical cancer treatment may include surgery, radiation, or chemotherapy, depending on the stage.
Follow-Up Care
If you receive an abnormal result, your healthcare provider will guide you and recommend the best course of action for your health.
Abnormalities can be treated effectively when detected early, preventing progression to cervical cancer. Your healthcare provider will tailor follow-up based on the severity of the abnormality and your medical history.
Regular Cervical Screening at Stella Mattina
Avoid an abnormal Pap smear and HPV! At Stella Mattina, we offer comprehensive Pap tests and HPV tests to detect abnormalities early – because cervical screening is the best way to prevent cervical cancer!
Schedule your Pap smear and HPV test today at your chosen location!
Dr. Krum is currently in practice in Arlington, TX. He received his undergraduate degree at Texas A&M University, then attended UTMB Galveston for medical school, finishing in 1986, completing his residency there in 1990. Providing a full range of obstetrical and gynecological care, he specializes in the treatment of endometriosis and robotic surgery. He arranges his schedule so that same-day appointments are usually available.