
Long, heavy, and painful periods? Or no periods at all? Might you have PCOS, you wonder? Or is it endometriosis? The idea of PCOS vs. endometriosis can be confusing before you have a diagnosis.
Polycystic ovary syndrome (PCOS) and endometriosis are two of the most common yet often misunderstood conditions affecting women’s reproductive health.
Both endometriosis and PCOS share overlapping symptoms – such as irregular periods and potential fertility challenges. But they’re fundamentally different in their root causes, risk factors, and treatments.
So, how to find out if you have endometriosis or polycystic ovary syndrome? How to differentiate and diagnose both conditions? And, above all, how to treat them? Is it possible to conceive and have a healthy pregnancy if you have either one of them?
If you suffer from PCOS or endometriosis, it’s only normal to have all those doubts, especially if children are in your plans.
Thinking of that, we gathered all the information you need in this ultimate guide about PCOS and endometriosis.
Table of contents
Understanding PCOS and Endometriosis
What is PCOS?
How PCOS Affects Your Fertility and Health
What is Endometriosis?
What are the Stages of Endometriosis?
How Endometriosis Affects Your Fertility and Health
How Do You Know Which Condition You Have – PCOS vs. Endometriosis?
How to Get Tested for PCOS and Endometriosis
Treatment for PCOS vs. Endometriosis
Understanding PCOS and Endometriosis
As mentioned, both PCOS and endometriosis are common gynecological conditions that can significantly impact your health and fertility. But they do so in different ways.
Polycystic ovarian syndrome is a hormonal disorder that affects ovulation and metabolism. Endometriosis is a condition where tissue similar to your uterine lining grows outside your uterus, leading to pain and potential structural complications.
Understanding how both endometriosis and PCOS affect your body is essential for:
- Managing symptoms
- Improving your quality of life
- Navigating fertility challenges
To help you out, here’s an overview of each condition and the key differences between them.
What is PCOS?
Polycystic ovary syndrome (PCOS) is a common hormonal disorder that affects ovaries, typically during a person’s reproductive years. It’s a condition that disrupts normal ovarian function and can lead to a variety of health complications, including infertility.
Despite the name, having PCOS doesn’t necessarily mean you have polycystic ovaries or ovarian cysts! Instead, the term “polycystic” refers to the ultrasound appearance of the ovaries rather than actual cyst formation.
So – the “cysts” in polycystic ovaries are actually underdeveloped follicles caused by disrupted ovulation, whereas true ovarian cysts are separate structures that can form for various reasons, including endometriosis.
Causes of PCOS
Though the exact cause of PCOS isn’t fully understood, several factors contribute to its development, including:
- Hormonal changes: PCOS disrupts the balance of reproductive hormones, particularly insulin, androgens, and progesterone.
- Insulin resistance: Many women with PCOS have difficulty processing insulin, leading to higher insulin levels. This can stimulate the ovaries to produce excess androgens.
- Genetics: PCOS often runs in families, which suggests a genetic component.
- Inflammation: Low-grade inflammation is linked to PCOS and may contribute to increased androgen production
Common PCOS Symptoms
PCOS symptoms present differently in each person, but the most common ones include:
- Irregular menstrual cycles or missed periods
- Difficulty with ovulation and fertility issues
- Weight gain, especially around the abdomen
- Excessive hair growth (hirsutism) on face, chest, or back
- Acne and oily skin
- Scalp hair thinning or hair loss
- Darkened skin patches (acanthosis nigricans), often on the neck or underarms
- Increased risk of metabolic conditions, such as type 2 diabetes, high cholesterol, and high blood pressure
How PCOS Affects Your Fertility and Health
One of the biggest challenges for people with PCOS is difficulty conceiving. This is mainly due to irregular or absent ovulation (anovulation). This can make it harder to predict or achieve pregnancy. But the effects of PCOS can be long-lasting and extend beyond reproductive health.
This is why PCOS requires ongoing management to reduce the risks of developing other long-term health conditions like diabetes, heart disease, high cholesterol, mood disorders, and endometrial cancer.
PCOS Impact on Fertility
- Irregular ovulation: Many women with PCOS do not ovulate regularly, reducing the chances of conception.
- Hormonal disorder: High levels of androgens can interfere with normal reproductive processes.
- Poor egg quality: Insulin resistance and inflammation associated with PCOS may affect egg development and quality.
- Thickened ovarian capsule: Some people with PCOS have a thickened outer layer of the ovary, which can make it harder for eggs to be released.
But don’t fret. While PCOS can make conception more challenging, you can still successfully become pregnant. Lifestyle changes, hormonal treatments, and in some cases, ovulation-inducing medications or assisted reproductive technologies (e.g., IVF, IUI) can all help you conceive.
Now, let’s understand endometriosis.
What is Endometriosis?
Endometriosis is a chronic condition where tissue similar to the lining of your endometrium grows outside the uterus. This misplaced tissue can grow on your ovaries, fallopian tubes, pelvic lining, and even in areas beyond your reproductive organs, such as the bladder or intestines.
Unlike the normal endometrial lining, which sheds during menstruation, endometriosis tissue has no way to exit your body. This can lead to inflammation, scarring, and chronic pelvic pain.
Causes of Endometriosis
The exact root cause of endometriosis is still unclear, but here are some possibilities:
- Retrograde menstruation: Some menstrual blood, containing endometrial cells, flows backward into your pelvis – reaching other organs – instead of leaving your body.
- Immune system dysfunction: Your body may fail to recognize and remove endometrial-like tissue growing outside the uterus.
- Hormonal disorder: Most people with endometriosis are estrogen-dominant, and estrogen plays a key role in the growth of endometriosis lesions.
- Genetic factors: Studies suggest that endometriosis occurs in families, suggesting a genetic predisposition.
- Surgical implantation: Surgeries like C-sections or hysterectomies might cause endometrial tissue to attach elsewhere in the body.
Common Endometriosis Symptoms
Endometriosis symptoms vary widely from person to person, but most people experience severe pain, especially during menstruation. Some common signs include:
- Intense or chronic pelvic pain (often mistaken for pelvic inflammatory disease)
- Painful periods
- Pain during or after sex
- Painful bowel movements or urination, especially during menstruation
- Irregular menstruation and heavy bleeding
- Infertility or difficulty conceiving
- Fatigue, bloating, nausea, or digestive issues (often mistaken for IBS)
What are the Stages of Endometriosis?
Endometriosis is classified into four stages based on the location, amount, depth, and spread of endometrial-like tissue – as well as the presence of scar tissue (adhesions) and ovarian cysts (endometriomas).
The staging system is based on the Revised American Society for Reproductive Medicine (rASRM) classification. But it doesn’t always correlate with symptom severity. This means even mild cases can cause severe pain, while advanced cases may be asymptomatic.
Here’s an overview of endometriosis stages:
Stage #1: Minimal
- Small, superficial lesions (implants) on your peritoneum (pelvic lining)
- Little to no scar tissue or adhesions
- Usually no significant ovarian involvement
- Symptoms may be mild or absent
Stage #2: Mild
- More lesions than in Stage 1, but still shallow
- Slightly deeper implants in the peritoneum
- Minimal scar tissue may begin to form
- Symptoms may include moderate pelvic pain or discomfort during periods
Stage #3: Moderate
- Numerous deep implants in the peritoneum and possibly on the ovaries
- Small ovarian cysts (endometriomas) may be present
- Adhesions (scar tissue) start forming, possibly affecting the fallopian tubes and ovaries
- Fertility issues may start to appear due to blocked fallopian tubes or ovarian involvement
- Symptoms can include moderate to severe pain, heavy bleeding, digestive issues, and more noticeable menstrual irregularities
Stage #4: Severe
- Extensive deep implants affecting multiple organs (e.g., ovaries, fallopian tubes, bladder, intestines)
- Large endometriomas (chocolate cysts) on the ovaries
- Dense adhesions perhaps causing organs to stick together (frozen pelvis)
- High likelihood of severe pain, heavy bleeding, infertility, and complications with digestion and urination
- Possible experience of chronic pain even outside of your menstrual cycle
How Endometriosis Affects Your Fertility and Health
Both endometriosis and PCOS are leading causes of infertility, affecting most women who are struggling to conceive. Endometriosis, specifically, can interfere with fertility in several ways:
- Adhesions and scar tissue may block the fallopian tubes or alter ovarian function.
- Chronic inflammation can make the uterus less receptive to implantation.
- You have reduced ovarian reserve or impaired egg development.
Beyond fertility, endometriosis can also affect your overall health, increasing the risk of chronic pain and fatigue, gastrointestinal issues, and depression and anxiety due to the chronic pain.
How Do You Know Which Condition You Have – PCOS vs. Endometriosis?
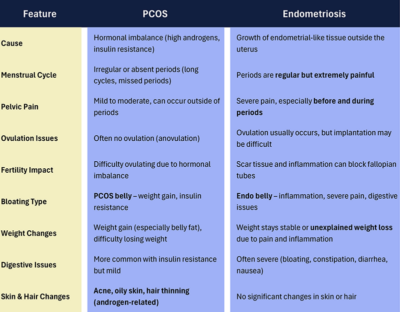
Since both endometriosis and PCOS can cause pelvic pain and irregular periods, it can be confusing to distinguish between them. But the key symptoms below can help identify which one you might have.
Symptom Overlap in Endometriosis and PCOS
1 Irregular periods.
2 Pelvic pain.
3 Hormonal imbalances (both conditions may be due to hormonal disorder, but PCOS involves androgen dominance, while endometriosis involves estrogen dominance).
4 Difficulty getting pregnant.
5 Physical body changes. Some women experience bloating and notice fat concentration in the abdominal area, known as PCOS belly and Endo’s belly. (However, PCOS belly is related to weight gain and insulin resistance, while Endo’s belly is due to inflammation, pain, and fluid buildup in the pelvic area).
How to Differentiate Between PCOS and Endometriosis
Below are the key differences between endometriosis and PCOS to help you identify which condition you may have:
Is PCOS or Endometriosis Worse for Fertility?
You must know by now that both PCOS and endometriosis can make it harder to conceive, affecting fertility in different ways. The impact depends on the severity of your condition, hormone levels, and how your reproductive system is affected.
So, the best way to avoid infertility is early diagnosis and management of endometriosis and PCOS – which brings us to the next topic: diagnosis!
How to Get Tested for PCOS and Endometriosis
Testing is essential to get the right diagnosis. However, endometriosis and PCOS require different types of evaluations, as follows…
PCOS:
Your doctors will use a combination of medical history, physical exams, blood tests, and imaging to diagnose PCOS. The main tests include:
- High androgens (testosterone, DHEA-S).
- LH & FSH ratio.
- Insulin and blood sugar.
- Thyroid & prolactin levels.
- Ultrasound to check your ovarian appearance and uterine lining.
A diagnosis of PCOS is only possible when at least two of the following three Rotterdam criteria are met:
- Irregular or absent ovulation
- High androgen levels (hyperandrogenism)
- Polycystic ovaries
Endometriosis
Endometriosis is harder to diagnose than PCOS because it doesn’t always show up on ultrasounds or blood tests.
Your doctor will start with a symptom assessment and pelvic exam to check if you experience pelvic pain, painful periods, digestion issues, and infertility struggles. A pelvic exam may also reveal tenderness, nodules, or cysts.
Then, they may opt to do a pelvic ultrasound and an MRI to check for endometriomas – but these are not 100% accurate in detecting all endometriosis tissue, as they don’t usually detect smaller lesions or adhesions.
For this reason, a laparoscopy is the ONLY definitive way to diagnose endometriosis.
A laparoscopy is a minimally invasive surgery where a small camera is inserted into your abdomen to look for endometrial tissue growing outside your uterus.
If endometriosis is found, doctors can remove or biopsy the tissue during the procedure.
 Treatment for PCOS vs. Endometriosis
Treatment for PCOS vs. Endometriosis
Both PCOS and endometriosis require different treatment approaches based on your symptoms, fertility goals, and overall health.
Neither condition has a cure, but managing symptoms effectively can improve your quality of life and reproductive health.
PCOS Treatment
Since PCOS is hormonally driven, treatment focuses on balancing hormones, regulating periods, and addressing metabolic issues, including:
- Lifestyle and diet changes
- Birth control pills to regulate cycles, reduce androgens, and improve skin
- Other medications, like Metformin to help with insulin resistance and weight management
- Anti-androgen medications (e.g. Spironolactone) to reduce excess hair growth and acne
- Fertility treatments like ovulation induction (Clomid, Letrozole) or in vitro fertilization (IVF), if other fertility treatments fail.
Endometriosis Treatment
Endometriosis treatment focuses on pain relief, hormone suppression, and surgical intervention if needed. Treatment may include:
- NSAIDs (Ibuprofen, Naproxen) to help relieve inflammation and pain
- Birth control pills to reduce estrogen stimulation and slow endometrial tissue growth
- GnRH Agonists (Lupron, Orilissa) to temporarily induce menopause-like hormone suppression to shrink endometriosis lesions
- Surgical treatment for severe cases (laparoscopy or hysterectomy as a last resort option)
Get Expert Care for PCOS and Endometriosis at Stella Mattina
Looking for a PCOS or endometriosis specialist near you? Look no further than Stella Mattina.
Living with endometriosis and PCOS can be challenging, but you don’t have to face it alone. At Stella Mattina, our gynecologists provide personalized diagnosis and treatment plans to help you manage symptoms – and (along with our obstetric specialists) help you conceive and have a healthy pregnancy.
Choose your nearest location and schedule an appointment today.
Dr. Krum is currently in practice in Arlington, TX. He received his undergraduate degree at Texas A&M University, then attended UTMB Galveston for medical school, finishing in 1986, completing his residency there in 1990. Providing a full range of obstetrical and gynecological care, he specializes in the treatment of endometriosis and robotic surgery. He arranges his schedule so that same-day appointments are usually available.




 Treatment for PCOS vs. Endometriosis
Treatment for PCOS vs. Endometriosis